Diabetic Retinopathy: Cause and Treatment.
Limiting the Effects of Diabetes of Your Vision.
What is diabetic retinopathy? The chemical changes caused by diabetes can damage blood vessels throughout the body, including the fine blood vessels in the retina, the seeing part of the eye. This damage is called diabetic retinopathy. There are two kinds:

Nonproliferative diabetic retinopathy (NPDR) happens when the retinal blood vessels start to leak, causing blood or fluid to seep into the retina. The retina becomes thick and swollen and does not work correctly. If the leakage happens in the macula (the central part of the retina) then vision will be blurred. If the leaks occur on the periphery of the retina, vision may not be affected.
Proliferative diabetic retinopathy (PDR) happens when the retinal blood vessels close, cutting off nutrition to the retinal tissue. Abnormal new blood vessels (called neovascularization) may cause bleeding and form scar tissue. If left untreated, the bleeding (called a vitreous hemorrhage because the blood fills the vitreous cavity inside the eye) and scar tissue can result in blindness. The earlier neovascularization is discovered, the better the chances are that surgery can save vision.
Both types of diabetic retinopathy can happen without a noticeable change in vision. If you have diabetes, it is critical that you have your retinas examined every six months by a retina specialist.
Diabetes affects 16 million Americans, and is the leading cause of new cases of blindness in people aged 20-74. Each year from 12,000-24,000 people will lose their sight from diabetes. Fortunately, vigilant care can markedly reduce the risk of visual complications from diabetes. For those who develop problems, new treatment technologies offer hope for saving and possibly recovering some sight.
What is diabetes?
Diabetes is a chronic disease where the body does not produce or properly use insulin, a hormone that helps convert sugar and food into energy. The resulting biochemical reactions can have a profound impact on the eyes. High sugar levels thicken the lens, which bends the light that filters through. When sugar levels decrease, the opposite occurs. The constant thickening and thinning of the lens due to dramatic swings in blood sugar levels leads to blurry vision. For people who are unaware that they have diabetes, blurry vision is often the first signal that something is wrong. For diagnosed diabetics, blurry vision is a warning to get blood sugar levels under control through a combination of diet, exercise and medication.
How is diabetic retinopathy treated?
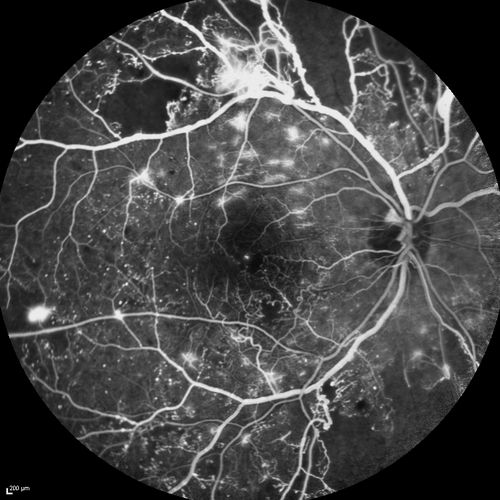
For patients with PDR, laser surgery and/or injections of anti-vascular endothelial growth factor into the eye can seal the blood vessels. This can stop the leaking and prevent further vision loss. Your doctor will perform a test called a fluorescein angiogram to pinpoint the exact locations of the leaks. In some cases, the diagnosis and treatment can be performed at the same visit. Even after surgery, new leaks may develop or sealed leaks may reopen, requiring additional treatment. This quick, relatively painless procedure can be done in one of our offices. That’s why it is important to check your vision each day and report any changes or blurriness to your doctor.
For patients who don’t respond to laser and/or injections, a vitrectomy can be performed in the operating room. This surgical technique removes the vitreous, the jelly-like substance in the center of they eye cavity. At that time, the doctor also removes any scar tissue that has formed. Eyesight gradually returns over the next six weeks. 90% of our patients who undergo this procedure enjoy a marked improvement in their vision, with some experiencing as much as 80% correction.